But What About Our Thoughts? Why Do We Obsess With OCD?
It may be surprising for you to learn that unwanted, intrusive thoughts are experienced by most people. A 1992 study carried out by researchers Christine Purdon and David A. Clark, examined the prevalence of intrusive thoughts in a non-clinical population. They listed 52 different potentially distressing thoughts, ranging from accidently leaving the stove on to stabbing a family member, and asked participants to rate whether or not they had experienced these thoughts. You can find a list of the thoughts, and percentages of people admitting to having experienced them here. They found that many of the participants had experienced, even quite potentially distressing, thoughts at some time. It’s important to remember here that this was a non-clinical sample. If we were to assume that the outcomes of this study were relatable to the wider population, we may believe that intrusive thoughts are a very common phenomenon.
So if intrusive thoughts are so common, why doesn’t everybody develop OCD?
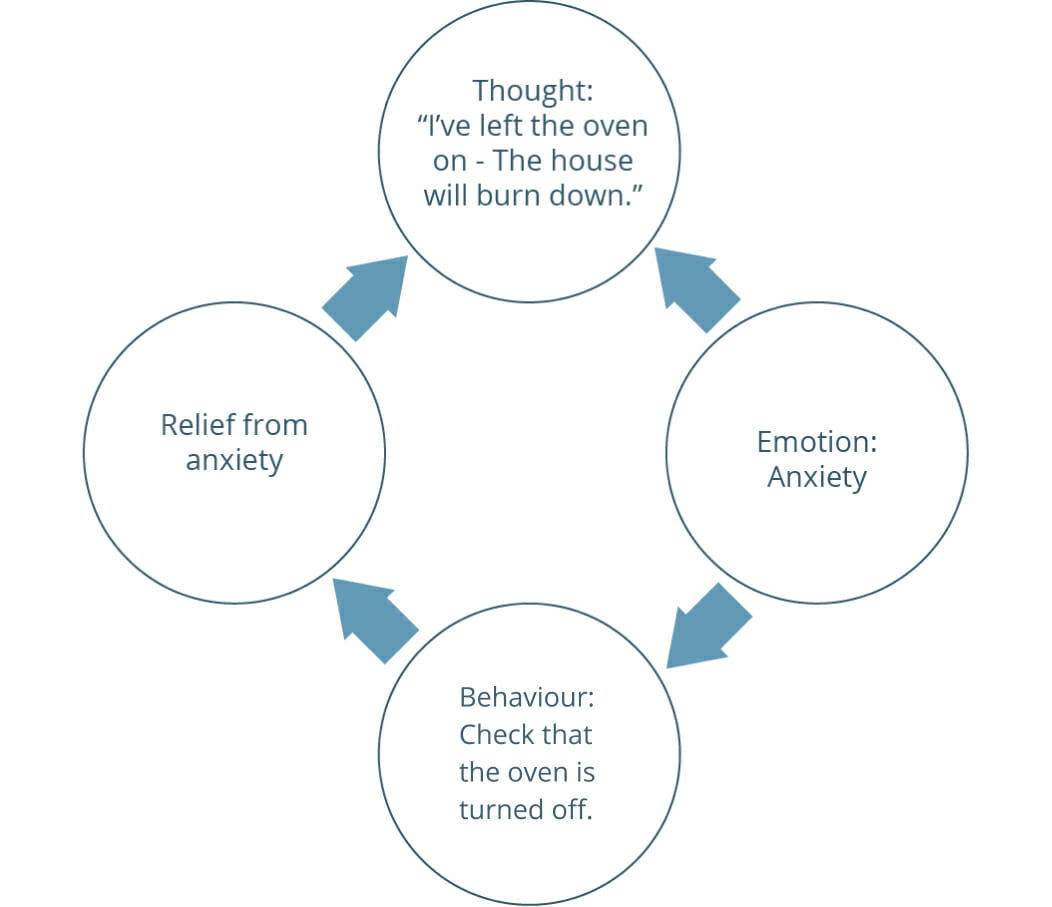
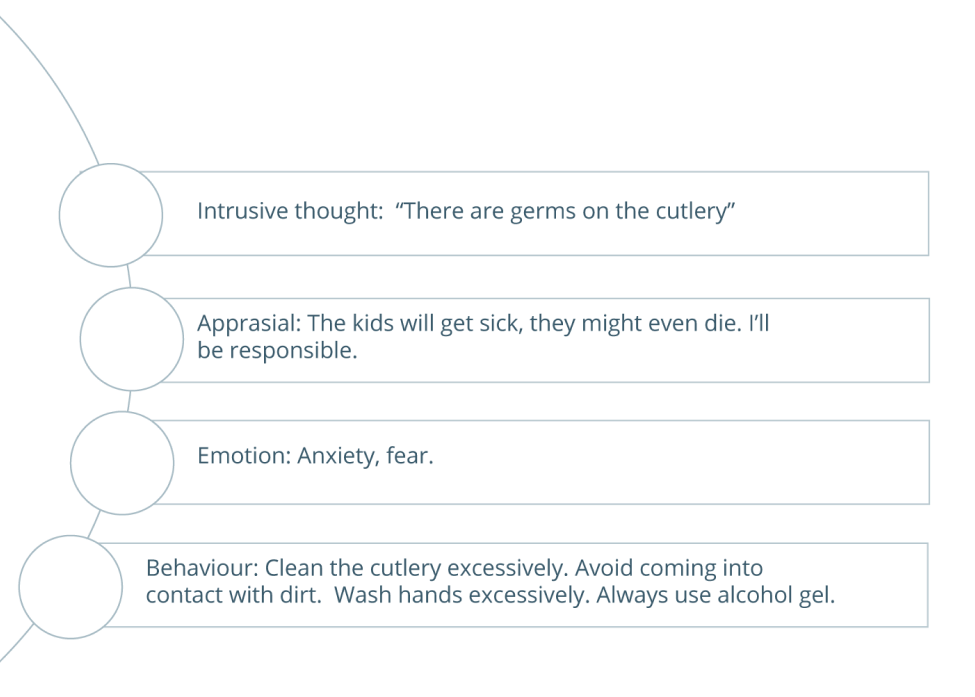
Many Cognitive Behavioural models of OCD suggest that it is not the intrusive thought itself which leads to the emotional distress, but the individual’s appraisal of it. We tend to find that people with OCD appraise the thought as potentially being indicative of a catastrophic occurrence actually happening, and that they have a high level of responsibility for this. This “inflated sense of responsibility” is a key ingredient of the OCD presentation and underpins the excesses that individuals will go to to prevent the feared event actually happening. Take a look at the diagram to understand this further.