Cognitive Behavioural Therapy(CBT) for Birth Trauma post-natal PTSD
Post-Natal PTSD caused by birth trauma is a problem that effects hundreds of families every year. A traumatic birth event can lead to the development of Trauma and post-natal PTSD symptoms and can also lead to post-natal depression symptoms in both women and men.
This article is part of a series exploring how post-natal PTSD symptoms caused by a traumatic birth event presents for families and highlights how it can be treated using Cognitive Behavioural Therapy.
- Self Help for PTSD Symptoms & Birth Trauma
- Understanding Your Response to Birth Trauma
- What Keeps Childbirth PTSD Symptoms Going?
- Birth Trauma & Post Natal PTSD
This section is going to focus upon what Cognitive Behavioural Therapy (CBT) for Birth Trauma Post-Natal PTSD looks like in practice, with a view to informing you about what to expect when you access help from a professional therapist.
Through experience, I have found that the quality and type of therapy delivered to individuals with post-natal problems can vary, and can deviate quite significantly from “best practice”. After reading through this article, and the following on EMDR for PTSD, you will know what to expect from “gold standard” treatment.
CBT and EMDR are the only two types of treatment recommended by the National Institute for Clinical Excellence for the treatment of PTSD in the UK. If you have PTSD, then you should have Trauma focused CBT or EMDR.
Again, this is presented for information purposes and it is always recommended that you access treatment from an accredited CBT or EMDR therapist. A good therapist will not only be able to deliver these techniques in an effective way, but will also make you feel safe, involved and supported throughout. This is vitally important as working through post-natal trauma symptoms in therapy effectively can often be an intense emotional journey.
Two CBT Models
Whilst there are other Trauma focused CBT ways of working I am going to introduce the two most widely used “models”. The first is what we call “Prolonged Exposure Treatment” and it was developed by Psychologists Edna Foa and Barbara Rothbaum .
The second model was developed by Anke Ehlers and David Clark and is largely what we would call a “Cognitive Model of PTSD”.
Prolonged exposure therapy for PTSD
I have covered earlier in this series about how PTSD symptoms are kept going by the individual trying to avoid thinking about the birth trauma event and also avoiding things that remind them of it.
This avoidance results in the trauma memory remaining raw and unprocessed by the brain. This means that when a memory is “triggered” it can feel emotionally overwhelming and can have the qualities of if it was happening all over again in the here and now, rather than in the past – we call this a flashback.
Basically, avoidance is what maintains PTSD symptoms.
Foa and Rothbaum’s prolonged exposure Treatment model works by teaching the client how to directly overcome this avoidance.
It’s important that your therapist is sufficiently skilled and is with you all the way.
Step 1 – Stress inoculation training
Because traumatic memories can by their very nature be distressing and emotionally overwhelming, it is vital the you are able to develop the skills with which to cope. To support this, Prolonged Exposure Treatment is typically accompanied by “Stress inoculation training”.
Stress inoculation has two main aims:
- To enable you to cope with symptoms between therapy sessions
- To enable you to cope with your distress during prolonged exposure in session
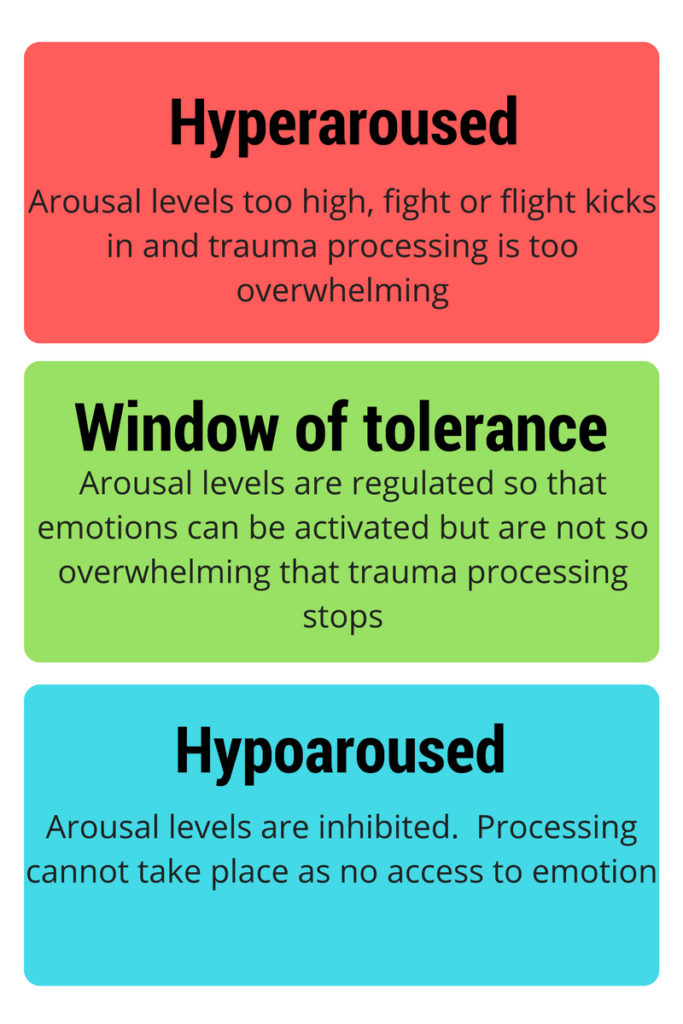
Stress inoculation can take the form of diaphragmatic breathing, breathing retraining or progressive muscle relaxation. Ideally we are aiming to give you the skills to regulate your distress to stay within what we call the “window of tolerance”.
The window of tolerance
The window of tolerance is an area of emotional intensity in which the client is able to feel the emotion associated with the memory of the trauma.
If the client becomes too emotionally aroused, that is, if it becomes too emotionally intense, then the fear response can feel overwhelming, leading the client to shut down the processing of the trauma memory.
Conversely, if the client is unable to generate any emotion in relation to the traumatic event, in that they may not be able to associate with it, then the processing can again not take place.
The client needs to be able to feel some degree of emotion, but be able to regulate themselves enough so that they do not become completely overwhelmed.
This middle bit – not too high, not too low, is our window of tolerance.
By using stress inoculation techniques, we are able to manage the levels of emotion during treatment and, as you become more used to using the techniques and as you engage more in the treatment plan, the window of tolerance actually becomes wider.
The more distress you can learn to tolerate, the more prepared you are to tolerate distress in future.

Step 2 – Prolonged Exposure to the Trauma Memory
After being trained in how to use the stress inoculation strategies, you will then be helped by your therapist to begin to be exposed to the avoided aspects of the trauma event.
This takes two forms:
- Exposure to the memory of the trauma event.
- Exposure to external triggers associated with trauma event.
As mentioned earlier, avoidance of thinking about the trauma memory can prevent the memory from being fully processed, leaving it “raw” and emotionally overwhelming whenever it is remembered in future. So, at this point in prolonged exposure treatment, the therapist will teach to how to be exposed to the trauma memory. Take a look at the graph below:
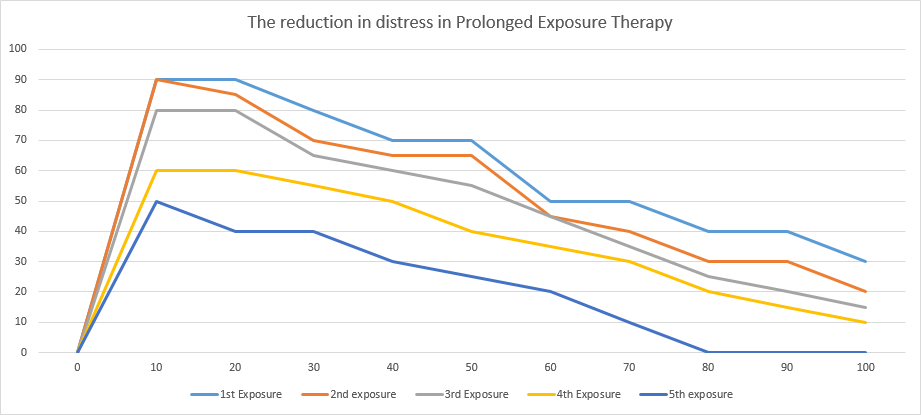
Here we can see what happens to the individual’s distress when they are exposed to the trauma event multiple times.
On the first exposure we can see that the highest level of distress is recorded at 90% – clearly very high!
But look what happens to the level of distress over the course of the prolonged exposure session…
We can see that the distress levels start to go down.
Now look at the levels on the 2nd, 3rd, 4th and 5th prolonged exposure sessions. The anxiety starts at a lower level each time, reduces more quickly and reduces to a lower overall level. This process of reducing distress by facing the feared memory head on for a prolonged period is called Habituation. We habituate to the feared memory and over time realise that we can not only tolerate the distress that it triggers, but also that it is nothing at all to be feared.
How your therapist will do prolonged exposure to the trauma memory
Ask you to close your eyes – if you feel really uncomfortable with this then you may keep them open (no one can force you to do anything that you don’t want to) but closing ones eyes can help you to really get in touch with the trauma memory.
Starting at the start of the traumatic memory, before anything “scary” had happened, begin to describe what happened. This should be done in the first person perspective, as though it was happening in the here and now. Your therapist will encourage you to describe as much sensory detail as you can remember – again, this is done so that you can really get in touch with the memory. Here’s an example:
So, I’m at home sitting in the living room. I can see the TV on and can hear my wife upstairs running herself a bath. It’s about six o’clock and the news is coming on. I can smell dinner getting cooked. Then I hear a louder splash and a groan coming from upstairs. I’m jumping up quickly and can feel my heart beating. ‘Somethings happening’, I think…
3. Continue in this way until you reach the peak of the distress in the trauma memory – This is called the “Hotspot”. At this point, your therapist will support you to really slow down and focus upon each aspect of the hotspot; sights, sounds, smells, thoughts, etc. This is so that you remain focused upon the event, can avoid very little and so habituation can take place.
4. Gradually you will continue to work your way through the trauma event, back to a point at which you feel safe again – “Start safe, end safe“.
5. Throughout this process, your therapist will have been asking you for ratings of your distress at regular (usually 10 minute) intervals. These ratings will be given as a percentage – high distress is a high percentage, low distress is a low percentage. We call these ratings “SUDS” which stand for “Subjective Units of Distress”. Your therapist will ask, “What are your SUDS now?” and then will record your response on a chart like the one above.
6. When you have completed one reliving of the trauma memory, the therapist will ask you to do it again, again following the procedure detailed above. Typically, a Prolonged exposure therapy session will last for up to 90 minutes and will consist of a number of relivings of the trauma memory. This is so that you have plenty of time to habituate to the trauma memory.
7. The session will ideally be recorded, on audio at the very least. This is so that you can take the recording away with you and repeat the prolonged exposure task by yourself at home as a between session task (there are lots of between session tasks in CBT!).
8. The therapist will also ask you, quite early on in therapy, to write out a detailed script of the trauma event. Again, the purpose of this is to get you used to the emotions associated with the memory and to help the brain process it. Again, this may seem quite daunting at first but there are so many benefits to this approach.
Step 3 – In-vivo Exposure
An important objective of any trauma focused therapy is to support you to “get your life back”.
Often, because of the combined effects of the symptoms of PTSD – the flashback, avoidance, nightmares and fear of something bad happening – the client’s life can change significantly. You may have taken a lot of time from work, stop spending time with friends or isolate yourself from family.
In-vivo exposure aims to support you to face head on the situational triggers that you currently avoid.
Using the same principles of habituation as detailed above in prolonged imaginal exposure, the therapist will support you to overcome your fears by exposing you to feared real-life situations. Again, just like with the imaginal exposure, habituation to these situations results in you losing your fears over time.
How your therapist will help you to do in vivo exposure
- Write a list of all of the situations that you currently avoid or feel a high level of fear in, as a result of it’s relationship to the initial trauma event.
- Decide which of these creates the most anxiety for you and which creates the least. Grade each of the other situations in terms of how much anxiety each creates for you. This is called a “Graded Hierarchy”.
- Now, starting with the least anxiety producing situation, your therapist will guide to to undertake your first in vivo exposure. Just like with imaginal exposure, you will face your fear for an extended period until your “SUDS” reduce by more that half of what they were initially.
- Repeat this procedure daily. The more you practice, the faster your recovery will be.
- Once you can tolerate one item on the Graded Hierarchy, move up to the next one and repeat the above process.
- Remember the golden rules for prolonged exposure: Exposure must be repeated, prolonged, graded and anxiety producing.
Cognitive Therapy (CBT) for Birth Trauma Post-Natal PTSD
The cognitive model of PTSD treats the trauma memory a little differently. Building upon Foa and Rothbaum’s PET model, the Cognitive model still involves an aspect of “reliving” the trauma in memory, but it does so with the aim of identifying unhelpful beliefs encoded within the memory and then updating them through further reliving.
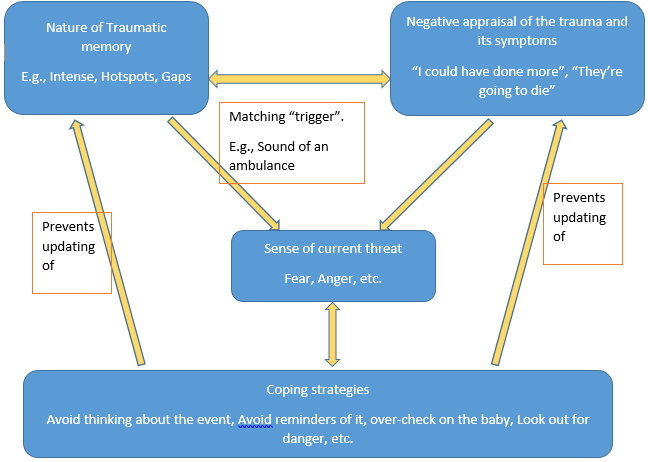
I’ve presented what the model looks like above. Lots of arrows and boxes, but please don’t get too hung up on this.
What these boxes and arrows show us are the different maintaining elements of PTSD. We have the nature of the traumatic memory itself, which may have some parts which are particularly overwhelming or it may have some gaps in the overall narrative. Your therapist will support you to develop this memory, through reliving and writing out what happened in the trauma event.
Next we have the box, “Negative appraisal of the trauma and its symptoms”. This is were we place the unhelpful beliefs that are encoded within the memory and also the changes in how we view the world after the trauma event.
When we are exposed to a “matching trigger”, something which reminds us of the traumatic event, we can see that it leads us to the next box labelled “sense of current threat”. This means that the memory and the thoughts we have about it combine to make us feel a sense of threat in the here and now.
At the bottom of the model, we can see the box labelled “Coping strategies”. This contains all of the things that we do to either reduce the sense of current threat or reduce other aspects of the PTSD symptoms. One example of a coping strategy is that, if the memory makes me feel a sense of current fear, then I will try to avoid thinking about it. Another might be to avoid “matching triggers” associated with the memory.
Following the arrows back up to the top of the model, we can see that the use of the coping strategies prevents the updating of both the nature of the memory itself (it remains incomplete, overwhelming and intrusive) and our beliefs about the trauma and its symptoms (I still should have done more, the world remains a threatening place).
How you will do Cognitive Therapy (CBT) for Birth Trauma Post-Natal PTSD
Your therapist will provide you with information about the symptoms of PTSD and about how it can be treated using Trauma focused CBT. They will then help you to understand the maintaining factors of your PTSD symptoms using the model presented above. This aspect of treatment is called “formulation“.
Then, to assist you in feeling confident in being able to tackle both working with the memory and doing the behavioural work necessary to get your life back, your therapist will show you how to manage your emotions using some of the self-help strategies for PTSD.
After this, the therapist will then support you to “relive” the trauma event. The CBT Therapist will again be looking for “Hotspots” in the memory and will be carefully looking for aspects of thinking which may be contributing to current levels of distress. For example, a father who witnesses his partner being hurried away to emergency care whilst in labour, may have a peak of distress at this point of the memory (a Hotspot). The CBT Therapist will seek to identify the negative thought at this point – e.g., “They’re going to die”.
After working with the client to develop cognitive restructuring skills, the therapist will ask the client to relive the memory again, but this time at the point of the hotspot where the client has the thought about his wife and child dying will ask, “What do you know now?”
The client will, whilst still vividly reliving the memory, be able to answer the therapist with new, updated information – e.g., “They’re both safe and well.” Understandably, this creates a different emotional response to the distress experienced previously.
You will also be asked to listen back to an audio recording of the session and to write out a detailed script of the event, this time including the new updated information.
By engaging in this process of reliving and updating, the client is able to enhance processing of the memory, discriminate between past and present interpretations of the trauma event and habituate to the memory, thereby reducing levels of distress when the memory is triggered naturally.
Again, just like with the Foa and Rothbaum PTSD model, the Ehlers and Clark PTSD model also has an emphasis upon enabling the client to “get their life back”.
This time however, the approach is based upon helping you to engaging in “behavioural experiments” to test out the reality of your trauma related beliefs in the real world. For instance the individual may have the thought, “If I don’t keep checking on my baby then something bad will happen”.
After using thought challenging techniques, which include the client identifying which of the unhelpful thinking styles that they are using (e.g., prediction, catastrophizing), along with developing alternative, more balanced thoughts, the therapist will help the client to develop an experiment to test out the thoughts.
This might be something like, instead of checking on the baby every 20 minutes, instead check on the baby after 30 minutes. The client would then be invited to return to their predicted negative thought and see if it truly was a realistic thought in light of the evidence gained from the experiment. Further experiments would continue to test out and modify these negative thoughts.
As the coping strategies are modified and reduced, the negative beliefs about the trauma and symptoms are able to be modified, leading to a reduction in current threat overall.
Conclusion
Here we have looked at how Cognitive Behavioural Therapy can effectively treat PTSD, Post-natal PTSD and Birth trauma related problems. The next section looks at how another treatment type, which is also recommended by NICE, can treat these symptoms. This treatment is called Eye Movement Desensitisation and Re-processing (EMDR).