Can EMDR help with Social Anxiety?
Eye movement desensitization and reprocessing (EMDR) is a type of therapy which has been shown to help PTSD, Childhood Trauma, OCD and other Anxiety Disorders.
But can EMDR help with Social Anxiety Disorder?
Here we will be taking a look at EMDR and how it can be applied to the treatment of Social Anxiety Disorder. I’m going to take you through some of the theory around EMDR and discuss how EMDR can help with Social Anxiety using a case example of how I successfully applied it to myself to cure my social anxiety.
How can EMDR treat Social Anxiety?
Social Anxiety Disorder is a recognised mental health problem in which an individual experiences an intense anxiety response when in social situations. If you have ever experienced it yourself, you will be familiar with the intense rush of fear, the seemingly inescapable self-consciousness and the desire to escape and hide from the situation.
EMDR has a proven track record for the treatment of anxiety based disorders. It works by activating the brains natural capacity for healing to unblock and process traumatic memories from our past that are affecting our lives today. “Bilateral stimulation”, in which visual (e.g., eye movements), auditory (bleeps) and Kinaesthetic (buzzers) stimulus is presented alternately is a key feature of EMDR therapy and heals by activating the left and right hemispheres of the brain, while we focus upon our traumatic memories.
Anxiety is our natural response to threat. So for us to have a socially anxious response, we are, often at a pre-conscious level, thinking that social situations are in some way threatening. This is what we term “a sense of social threat.” We believe that we will be be shamed, humiliated, embarrassed or rejected within the social situation, which activates our threat response. This activates all of our physiological responses to danger – increased heartrate, increased temperature, dizziness, shaking, breathlessness – and we, fearing that others will notice our anxiousness and therefore contribute to the risk of us feeling shamed, humiliated, embarrassed etc, turn our attention inwards. We scan our body for any indications that we are coming across as awkward, anxious or weak but, as we are only focusing on how anxious we feel, fail to find out if other people are noticing our anxiety.
While Cognitive Behavioural Therapy has been shown to be an effective treatment for Social Anxiety Disorder, with it being a “here and now” type of therapy, it’s focus on the origins of the problem for an individual are relatively minimal. This is where EMDR comes in.
EMDR can treat social anxiety by helping us to identify the origins of our social anxiety problems and work on the difficult memories of these events which are being activated (either at the levels of thoughts, images, emotions or physical feelings) when we are socially anxious. In essence, EMDR targets the early experiences that made us develop the sense of social threat in the first place.
Memories are activated by triggers. When I am exposed to a trigger that reminds me of a traumatic or otherwise emotionally difficult experience in my life, the memory can be activated. Often, when an event in our lives has been so emotionally difficult that to even think about it causes us intense emotions in the here and now, we might consider this memory to be unprocessed or blocked. EMDR can then be used as a way of unblocking the memory, meaning that when the newly processed memory gets activated by a trigger, we no longer experience the intense, raw emotion originally associated with the event. We can then live our lives without avoiding or fearing our traumatic memories being triggered.
Based upon this idea, we would then suggest that by processing earlier life experiences in which we experienced shame, embarrassment, fear or humiliation in a social situation (e.g., being bullied, singled out for criticism and abuse) to a degree that they no longer effect us, then we would be able to relieve social anxiety in the present. The triggers activate memories that no longer cause us distress. This allows us to remain present in the social situation and even have the opportunity to access more positive social experiences, further weakening the sense of social threat.
How can early experiences cause Social Anxiety?
The emotion of Anxiety is our natural response to threat and gives us the physical resources to cope with immediate danger. “Fight or Flight” are examples of two of the physical responses that are activated when danger is present. A commonly presented example of how fight or flight responses are helpful is what happens if we were faced by a predator, a lion, for example. As we see this threat, in mere seconds our mind and body work together to activate a whole system of physiological responses which help us to fight the lion or escape from it (flight).
But clearly, we are rarely being exposed to large predators when our social anxiety disorder is being activated, and yet all of the same physiological reactions are taking place. We feel tense, hot, shaky, and dizzy with a pounding heart – we want to escape or just do anything to get the attention away from us. Why does this happen?
As highlighted earlier, we are viewing social situations as though they are a threat. The social situation is essentially our Lion. But we also generally also have the insight, when we are not in the social situation, that the real threat is significantly less than this. We know that our reaction is excessive. At some level, at some time in our lives we have made an association through experience that social situations are capable of a threat towards us.
In my work with socially anxious clients, in addition to understanding the maintaining aspects of their problem – their unhelpful thoughts, their avoidance and safety behaviours – I am also keen to understand what early experiences have led to the problem development. Here are some typical themes that emerge:
- Bullying
- Emotional, physical and sexual abuse
- Neglect
- Narcissistic parenting
- Isolation
- Humiliation – e.g., being shamed for poor performance at school or at sports.
Personality types also play a factor however whether they are directly a cause of the social anxiety, or something which invites some of the above negative experiences is an issue of debate. For instance, introversion is largely an inherited personality trait. However, introversion, particularly in our “He who shouts loudest” society, can be viewed as a negative personality trait which can lead some children to be ignored, neglected or the target of bullying.
With the above taken into account, we can see how the associations between social situations and threat can develop, both at the conscious and the unconscious level. One of the real strengths of EMDR is that we are not only interested in obvious links. Often, particularly in relation to early life memories, memories of events are also manifested at the emotional and physical levels.
For the remainder of this article, I’m going to take you through how I used self-administered EMDR to near 100% cure my social anxiety problems. I can’t stress enough how much this approach has worked for me but I do need to add the obvious caveat: Don’t try self-administered EMDR at home. Please get help from a fully qualified, and preferably accredited EMDR professional. You can contact me and other suitably qualified EMDR therapists at the EMDR Association for UK and Ireland.
How I cured my social anxiety using EMDR
My social anxiety had been present from about 14 or 15 – I’ll go into all of the events that contributed to this later. Some people thought I was quiet, others sometimes ignorant and aloof but when at it’s worst, my social anxiety was almost crippling. It was like I just couldn’t actually get words out of my mouth or give eye contact in case something “bad” happened.
I can think of whole phases of my life when I was peripheral to the broader social situation, standing in the back or in the corner, allowing my closer friends who I felt comfortable with do all of the talking. I was a third wheel.
I could come out of my shell in some situations, but these usually involved drink, weed or putting on a sort of “I don’t care if you like me” aloof persona. With my CBT hat on, I see that all of these things were just “safety behaviours”, sticking plaster strategies that got me through in the short term, but became something that I relied upon.
As I got older, it affected me in lots of different ways. I’ve been through whole relationships where I couldn’t speak to the family members of friends or girlfriends. I’ve avoided the eye contact of countless bosses and not spoke up in meetings when I knew how things were going wrong. I’ve bought lots of wrongly fitting clothes which I’ve not been brave enough to take back to the shop.
I really don’t know how I’ve managed to get this far.
I’ve presented how I treated myself below in relation to the EMDR standard “8 Phase” protocol although I do also use some of the less technical language advocated by Laurel Parnell interchangeably. EMDR, whilst being a standardised, evidence-based, mode of treatment, also relies a lot upon the intuition of both the client and therapist. This is reflected in the steps I present below.
Step 1 – History taking
I had a pretty solid idea of the main events that led to my social anxiety.
I went to a pretty rough school in a rough area. The school’s highest wish for students was to not end up on benefits and I was bullied to various degrees throughout. I didn’t like school. As I was working through the history taking phase, I wrote down the more significant bullying events which may have contributed to my social anxiety and were therefore potential targets for EMDR processing. These bullying events contributed to a belief that I stood out for some reason, and that standing out leads to physical and verbal abuse. Thanks School!
Being aware that EMDR sometimes links current problems to memories that are not always obvious or conscious, I also needed to investigate what other events my brain associated to my current social anxiety problem. To do this I used an Affect Bridge, also sometimes called a Floatback.
The Affect Bridge simply invites your brain to trace back a current problem to earlier memories in which you experienced a similar emotion and/or belief. There were a number of events which came up for me, three of which related to a bullying, physically abusive headmaster I had had whilst at primary School. I’d always held a resentment towards this man but the three memories that came up for me, two of which I’d largely forgotten about, highlighted the huge effects that his behaviour towards me had had upon how I view myself and other people, particularly those in potential authority.
My targets for processing are presented here, using a Formulation presentation style based on that developed by Laurel Parnell.

I was going to start with the early “touchstone” memories. There were 3 which were relevant and all of which occurred in within a relatively close timeframe.
Interestingly, as I write this I can see that they all happened around the ages of 7 and 8, which is a key point in child development as the child starts to construct their view of themselves within the world. At this age, we are “Ego-centric” meaning that we are literally the centre of our own universe and tend to internalise external events as being attributed to us.
We have the 3 memories all relating to the bullying head master.
- The first in which he selected me as being someone who had beaten up another pupil and roared at me in his room until I confessed. I hadn’t even been near the other pupil – I was being forced to admit to something I hadn’t done.
- My mum being at the school (justly) complaining about me being blamed. The teacher had hit me and was denying it in front on my mum. I still ended up with a week of detentions.
- Being in a school assembly and the same teacher shouting out another boy for misbehaving and calling him by my name.
We have three early memories of being punished and implicated in things that we have absolutely no part in. The child (little me) obviously felt helpless, vulnerable in the sense that I was being punished for things I’d not done and fearful – this person had even got past the protection of my mum.
So how does this then relate to me being too scared to speak up in meetings?
As I said, senior school was hard. The earlier experiences at my primary school did however appear to contribute to how I approached the senior school. I was quiet, unconfident and wore my timidity across my face. This stood out to the other children starting on day one, when some kids were laughing as my name got called out from the register – “George”. Literally, my name invited shame.
It was a tough school and there were countless episodes in which I seemed to attract attention which led to bullying, fights and verbal abuse. Sometimes I fought back, sometimes I ducked out. For EMDR purposes, I treated these memories a a “cluster”, choosing an image that linked them altogether so that I could allow the brain to process them as a group – there were literally too many events to list individually. I chose the image of an event in which I was assaulted, cowardly and without any warning or justification, by a lad I didn’t even know who then proceeded to kick and punch me as I protected myself in the corner.
Another memory of which I am especially proud (/s) which the affect bridge brought up for me was when I was in my first year of senior school and I asked the teacher could I go to the toilet. She said no. Whereas some of the other more mouthy kids might have insisted that they were “about to go” and that going to the toilet was non-negotiable, I returned to my seat and held on…
…For a bit…
Rather than challenge the teacher, my mind hatched the plan to let out a bit of piss bit by bit and no one would ever notice.
Of course, they did. So this memory of being laughed at and ridiculed by a gang of feral kids because I was too scared to challenge the teacher became another catalyst for the development of my social anxiety and a target for EMDR processing. Even as a 41 year old man, I still have pangs of shame as I write this for a public forum. Please don’t judge.
It’s also interesting here to point out the connection in my emotional responses to teachers. Although the teacher in the urine incident was (aside from her need to prevent children from emptying their bladders) actually quite nice, in my mind a connection had been made between the way in the way I relate to teachers, and later more general “authority figures.” “Teachers/authority figures are threatening, humiliating and unfairly punitive.”
Lastly, we have a memory of an episode of having a social anxiety attack while at University, doing my CBT training no less. That “round robin” task that facilitators like to do – go around the room and everybody has to say something. As the lecturer was going around the group, my mind started to focus upon the thought of not being able to get my words out, looking stupid and being judged by the rest of the students. I tried to stay in the situation and to stay calm but the intensity of fear was too great and I had to leave the room. My image of this memory is looking in the mirror in the toilet, sweaty and pale wondering what had just happened.
In this incident the lecturer was a far cry from the kid-whacking bully of a headmaster from primary school, but there remains a theme running through the events. I was in a public situation, there was an authority figure present and I was about to be “chosen.”
Based upon the EMDR formulation presented above, I decided the I was going to focus initially upon the three early memories which had all happened relatively close together. I struggled to find anything earlier than this (at this stage) that may have contributed to the onset of the fears.
Step 2: Tapping in resources
Tapping in resources in attachment focused EMDR is used to give you the inner resources needed to feel prepared to “dip your toes” into the traumatic memories. Because a traumatic memory is typically not fully processed, it can often make us feel anxious and fearful about sitting with the memory and allowing EMDR to do it’s work. By building up resources before we start the work, we are better prepared to do the work necessary.
Tapping in in EMDR fulfils two main processes:
- We are creating resources which we can use during processing as “Resource interweaves.” More on this in a bit.
- We are broadening our Window of Tolerance. This diagram shows us the Window of Tolerance model.
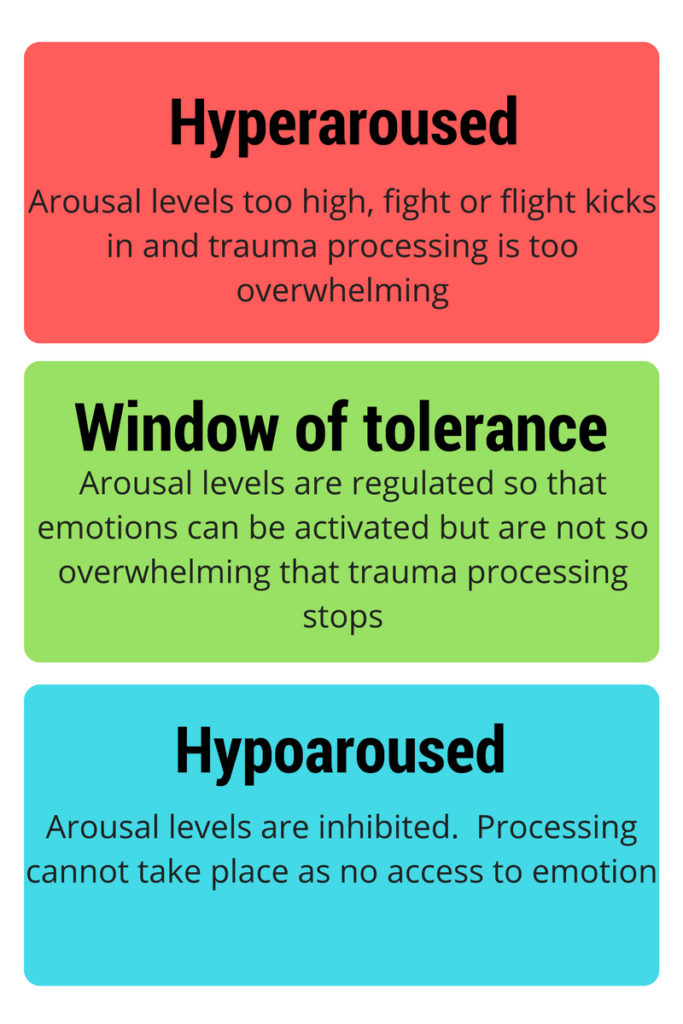
As you can see, there is a specific window in which we are able to tolerate the emotional distress associated with our trauma memories. If the memory is too emotionally intense for us, then we become “hyperaroused” and there is a possibility that we will not be able to sit with the trauma, and potentially dissociate from the processing. We don’t want this to happen because we want to keep the conscious brain “on-line” so that adaptive information can be integrated with the trauma memory.
If arousal levels are too low, then we are in a “hypoaroused” state. This means that our levels of emotional arousal are reduced and full emotional processing can’t take place as we are not with the full content of the memory.
Resource interweaves can also be used in a more active way in actually facilitating the adaptive information processing required to unblock our difficult memory.
In her Attachment-focused EMDR approach, Laurel Parnell supports generating a resource “team”. This takes the form of one or more people (real or fictional), animals or icons which can be called upon during EMDR processing to provide a resource as and when needed. Of course we know logically that the person or animal that we use in not actually there but we are again tapping into the minds incredible capacity to heal itself. As far as your mind is concerned, tapping into the imaginal presence of your resource team is as good as them being there.
I chose three members for my “team”, one nurturing/caring, one who is protective and one who I would call upon for wisdom. I’ll get into a lot more detail on tapping in in EMDR in another article, but for now I had my resource team and I gently tapped each of them in with short sets of EMDR bilateral stimulation using my buzzers and headphones.
Step 3: Assessment
Assessment in EMDR is not what you might think if you have had any sort of therapy before. It isn’t a diagnostic or clinical assessment. Instead, it is a process in which we aim to “light up” the target memory, bringing it to awareness and ready for us to work with it.
We activate the memory in a special way which lights up all aspects of memory in terms of imagery, thoughts, emotions and sensations in the body. We also want to establish at this stage what we would like to believe differently about ourselves in relation to the memory. Memories are not stored in discrete locations in the brain but are instead stored as a constellation of parts throughout – this Assessment stage of EMDR aims to get all parts of that memory online.
Starting with the memory of the headmaster shouting at me, this is what the Assessment of the memory looked like:
Image: Me, small and in tears and being shouted at by this big scary man, until I confessed to something I didn’t do.
Negative cognition (what do I believe about myself when this memory is activated?): “I’m trapped.” There were other negative beliefs about myself that came up including, “I’m weak” and “I’m helpless” but the negative thought about being trapped was the one that generated the most distress for me.
Positive cognition (What would you like to believe instead?): My immediate thoughts when working through this were, “I’m ok now”, but this felt like too general a cognition to work on. Instead I settled on, “I’m safe.”
Validity of cognition (VoC; with the Image of myself being shouted at in my mind I held the positive belief “I’m safe” there also. I then checked to see how believable this felt to me, at that moment, at the gut level). The VoC is rated on a 1 to 7 scale with 7 being complete belief in the thought. I rated my belief at 3 out of 7.
Emotion: It’s important to stress that this is how you feel right now, when the memory and negative thought are there in your mind, not how you felt back then. I know logically that I was obviously scared then, but it’s more important for us to understand how remembering the event feels to me today. When I accessed this memory, my emotions were mostly Fear and some sadness.
Subjective units of Distress (SUDS): SUDS are just a simple scale to help us identify the intensity of our emotional state. 10 is as high as it could be, 0 means none at all. For me, I rated it at 8 out of 10 for intensity.
Body: “The Body keeps the score” by Bessell van der Kolk is a famous text in the trauma literature. It relates to the idea of “body memory” and is particularly relevant when we are talking about memories of events that happened in childhood due to the fact that children do not always remember events in a narrative, word-based way. Instead, memories are often symbolic, visual, emotional and sensory. Therefore, to ensure that we are lighting up the full memory network, we also need to find out where the trauma is held in the body. In my case, It was feeling at it’s most intense in my legs and stomach.
Step 4: Desensitisation
Once the memory has been lit up, the bilateral stimulation begins. For me, I find it easiest to do EMDR with my eyes closed and use buzzers and headphones to provide the bilateral stimulation – of course this depends on the individual but I find it a little bit easier to stay with the imagery with my eyes closed.
There are lots of different metaphors which we use to illustrate the kind of observer stance that we are wanting the client to see when they experience EMDR processing. For instance, we might suggest that it’s like sitting on a train and watching all of the scenery (the images, thoughts, feelings and sensations) passing by. Alternatively, we might suggest that its like watching a TV or Cinema screen, the client sitting in their seat while the “movie” of the trauma memory plays out. The main principle that we are trying to illustrate using metaphors such as these is that the experience of EMDR requires us to observe whatever comes up, without us trying to want something to happen or stop memories from coming up. By adopting this observer stance, we are able to allow the brain to do it’s thing and fire up the whole of that troublesome memory network so that it can make new connections to more helpful, adaptive memories.
So, what is EMDR processing actually like?
First off, it’s different for everyone. There are no rights or wrongs but we often tend to see a series of new images, feelings thoughts and sensations come in and out of our experience. To describe the general experience, I often say to my clients that it’s like dreaming whilst awake.
Here’s what I experienced.
It takes a couple of sets of bilateral stimulation (bls) to get things going. As I focus upon the image, thoughts and feelings of the memory of being shouted at (and hit) by the headmaster, I start to notice other aspects of the event.
My mind drifts over to what happened just before I was blamed as the perpetrator of the attack on the other pupil, just innocently watching the teacher’s investigation and then the resultant shock and fear I felt when he decided that I must be the culprit. He made this judgement based upon the fact that the real perpetrator had a blue coat and I too had a blue coat. Top draw elimination from this guy.
…I do another set of BLS…
My mind then returned to the image of me standing there being shouted at. His words telling me that I had attacked the boy were getting louder and louder and seeming to be never ending. As I did this, I could vividly recall the spittle and froth from this increasingly incandescent giant landing on my face as I felt more and more helpless and fearful. Then I remember my “confession”. I re-experienced the words, “I did it” coming through a sobbing and shaking 7-year olds mouth. I then started to feel angry as he, rather than having the insight to realise that he had just terrified a kid into confessing to something that he hadn’t done, began to shout even more about how I had lied.
I’d love to meet this bully today.
…more BLS…
Another part of the event then came into my mind, (target 2 on the model shown earlier) mind just making the association by itself. After he had told me that I was a horrible boy and was going to lose my breaktimes for a week, he slyly whacked me in the back as he marched me back to class. Hard, aggressive and not the type of thing that you do to a 7-year-old (or anyone). A covert, sinister dig to a child as it’s back was turned and while no other adults were around; cowardly and with a hint that he would do more if he could.
I began to feel tearful.
The memory then shifted to me being tearfully walked back to the school by my mum after I told her what had happened, and then an image of her and him talking as he denied that he had hit me. I watched as he doublespoke the narrative into me just being scared of him hitting me when I have my breakdown detention. He looked at me and said, “are you scared that I’m going to thump you?” He was firm and insistent that I had done the crime and that I would be punished. Despite my mum being there for me, this man had even manipulated her. I was helpless.
Then came the first bit of adaptive information processing and a little more insight into the context of what was going on for me at the time which may have contributed my feelings of helplessness. My mind shifted to a memory of me being in a park with my dad and I was on a climbing frame explaining what had happened. My Dad was angry and wanted to go to the school and have it out with this Headteacher. I can remember him showing his teeth and clenching his fists as he listened to my story. It then dawned on me that at the time that this event occurred, we were midway through a house move and my Mum, my brothers and I were living at my Mum’s parents, while my Dad was living at his parents. This was purely for practical reasons while we waited for the new house to become available, but I wonder how this degree of upheaval at home would have contributed to my processing of the event at the time.
I then remembered that, even though we were going through this upheaval, I did feel safe when I thought about my family being there for me at the time. I probably did want my Dad to go into school and beat up the teacher and he probably wanted to do this too. I noticed a downward shift in my distress as I remembered that despite what was going on at school, my family definitely had my back.
…I continued with the BLS…
As this link between the “bad memory” and the knowledge that I had people there for me was made, other more positive associations began to come up. I remember how the wider family were supportive of us that summer, and a standout memory of being able to hear Michael Jackson’s Aintree concert from the doorstep of my Nan’s house. “Dirty Diana” to be specific.
After around 20 to 30 minutes of EMDR I had started to feel better.
I returned to the target memory that I had begun with – being shouted at – and again accessed the image that represented the worst part of the event. I re-rated my SUDS. 4 out of 10, a reduction of 50%, which was great but I wanted to get this all the way down to 0 or 1. I carried on.
The idea is that we allow the associations to the memory to work through “channels”. Each channel carries the memory down a different path of associations, loosening it up and linking it to other, more balanced and adaptive information as it goes.
Subsequent channels related to this memory took me down some other long forgotten paths. The thing about EMDR is that we don’t know where the brain is going to take us, we just have to go along for the ride – this is what makes it so unique and powerful. Memories of being chosen to be the nurse in a pre-school game of “Farmer wants a wife”, and then being laughed at as my gender-stereotyped 3 year old self protested with, “but I’m not a girl.” Authority, exposure and then shame. This theme runs throughout all of the negative memories that came up.
I repeated this process of BLS and brief pauses until the distress I associated with the target image had reduced all the way down to 0, which took about two one-hour long sessions of self-administered EMDR. Next, I need to work on the “Installation” phase.
Step 5: Installation
I mentioned earlier the phrase, “adaptive information processing.” This is the name given to how EMDR allows a blocked, unprocessed memory to make new connections with more balanced, resourceful and complete parts of our inner world.
The installation phase, in which we directly link our newly desensitised memory with a more balanced positive belief about ourselves, is an important stage in adaptive information processing. Here we call upon either our previously identified “positive cognition” from the assessment phase – mine was “I’m safe” – or we decide upon a new one which may have arisen during desensitisation which we now feel is more appropriate.
This phase is typically a lot quicker than desensitisation. We begin by again bringing up our memory of the event that we are processing. Then, if I was doing this with a client, I would ask “what do you believe about yourself now?” This might lead to them bringing up the previously agreed positive cognition or they may come up with another. Then, we re-take our “Validity of Cognition (VoC)”, which is if you remember a scale for rating how believable a belief is for us in relation to the memory that we are working on. This is rated on a 1 to 7 scale – 1 being not believable whatsoever, 7 being completely believable.
Holding both the memory/image of the event and the positive cognition, we will then use BLS to pair them together with our gauge of success being our validity of cognition scale which should gradually shift up to 7 out of 7.
When I did this on myself, it went through pretty quickly. I believe that this was due to the amount of care that had gone into the desensitisation phase. If we find that the installation becomes stuck in any way, it may be the case that there is something that makes the new positive cognition unbelievable in relation to the memory. In this case we can either:
- Return to the desensitisation phase and see if there are any unprocessed aspects of memory which are causing a block.
- Consider a different, perhaps more believable Positive Cognition
- Consider and develop other internal or external resources that may help the positive cognition to become more believable in relation to the memory.
Once I was satisfied that I had arrived at the point in which the positive cognition “I’m safe” was entirely believable to me in relation to the target I was processing, I moved onto the next phase – The Body Scan.
So, what were the effects?
Whereas in other therapies such as CBT in which we are quite specific about what our treatment goals are and we measure our treatment success in specific ways (e.g., To be able to hold a conversation with a stranger for 15 minutes with no safety behaviours with only 30% anxiety), we typically
For the day or two after I had done this work on myself, I felt as though I had been “cleansed” in some way. There is a strange comfort in having visited and worked through some of your deepest, long forgotten childhood experiences. There’s a nostalgia and a warmth to it, even when the memories that we begin with are distressing to us. The brain starts to make the connections between the trauma memories and the more pleasant, adaptive ones. We don’t just “know” at a mental level that we are safe now and able to move on with our lives, but we actually feel it.
There is a bit of a sadness too. Not a depressed, hopeless type of sadness. I felt for the child that was experiencing this upset. The powerlessness and the intimidation. But I also was able to reflect upon these experiences and relate them to the man I am today. These experiences, the bullying, the tough environment and wanting to make sense of myself in relation to these uncontrollable experiences are probably a big contributor to me having chosen to become a Psychotherapist.
In terms of my social anxiety symptoms, it may seem hard to believe but they simply…stopped. It wasn’t like I noticed anything particularly dramatic. I simply noticed one day that the things that used to trigger my fear, just didn’t. I really didn’t fear meetings anymore and even found it hard to care about what people thought about me in them. My wife has commented upon how I’ll just start up conversations with people and not seem even bothered about who it is I talk to. Not a conscious effort, but something that feels natural like I feel comfortable in my own skin.
In conclusion, Can EMDR Help with Social Anxiety? Yes, it really can!


